- 859-554-7360
- info@patientchoiceultrasound.com
- Mon - Fri: 8:30am - 5pm
Services
What is thermography??
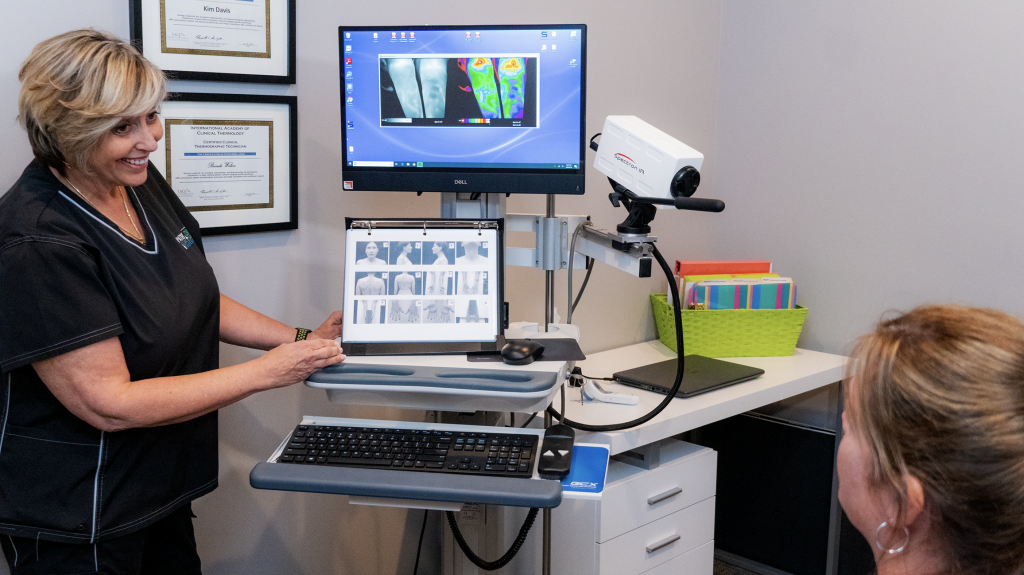
 Thermography, or infrared imaging, entails the use of specialized cameras that are sensitive to the detection of electromagnetic energy (light) in the infrared wavelengths (heat). As such, these imagers serve as a remote sensing system; nothing touches or harms the object under investigation. When the camera’s detectors sense the incoming infrared heat an electrical signal is produced that generates a visible image display.
Thermography, or infrared imaging, entails the use of specialized cameras that are sensitive to the detection of electromagnetic energy (light) in the infrared wavelengths (heat). As such, these imagers serve as a remote sensing system; nothing touches or harms the object under investigation. When the camera’s detectors sense the incoming infrared heat an electrical signal is produced that generates a visible image display.
Medical infrared imaging (MIR) entails the use of high-resolution infrared cameras and sophisticated computer processing to produce a topographic heat map display which bears a resemblance to the visible image of the body. Modern computerized thermography produces an accurate and reproducible high-resolution image that can be analyzed both qualitatively and
quantitatively for minute changes in skin surface heat emissions.
Is thermography covered by insurance?
Thermography is not covered by insurance. You may want to Check your voluntary insurance such as Aflac, and Colonial. Patient Choice Ultrasound and Thermography does accept Health Savings Accounts. All fees include the interpretation.
What do You need To Know before your exam? Including preparations!
- No prolonged sun exposure or tanning beds (especially sunburns) to the body areas being imaged 5 days prior to the exam.
- No used of deodorants, lotions, creams, powders, or makeup (no facial makeup for full body or upper body scans) the day of the exam.
- No shaving of the areas to be imaged the day of the exam.
- No treatment (chiropractic, acupuncture, TENS, physical therapy, electrical muscle stimulation, ultrasound, hot or cold pack use or physical stimulation of the areas to be imaged for 24 hours before the exam.
- If bathing, it must be no closer than 1 hour before the exam.
- If you are using pain medications, please avoid taking them for 4 hours prior to the exam. (YOU MUST CONSULT WITH THE PRESCRIBING PHYSICIAN FOR THEIR CONSENT PRIOR TO ANY CHANGE IN MEDICATION ).
- You must wait at least 4 weeks after having a fine needle or core biopsy of the breast before a thermogram can be performed.
- You must wait at least 8 weeks after having a lumpectomy or surgical biopsy of the breast before a thermogram can be performed.
- If you have had any surgical procedure within the last 12 weeks, please notify our office before coming in for your appointment.
- For breast thermogram-if you are nursing please try to nurse as far from 1 hour prior to exam as possible.
- No jewelry.
- Hair off face and off shoulders.
- Please be advised you will be asked to disrobe for your study. (All clothing interferes with imaging).
- If you have a thong please bring for your appointment. (Disposable are available).
Do I Need A Thermogram Follow-up? Why and When?
I’ve heard that after an initial thermogram the patient will need to return in 3 months for another thermogram so that a stable baseline can be established.
This is absolutely unnecessary! The argument for this practice seems to be that there is no way to know on your first thermogram whether or not your body was changing at the time. I have a question, if the follow-up 3 month thermogram showed that there was change, which image set would be the stable baseline? Would it be the first set or the 3 month later set? It sounds like you would need to do another set of images in another 3 months as a tie breaker. But what if this set also showed change? The bottom line is that if you did need to return to do any of this the technology must be useless.
What would you think if your doctor took your temperature, noted it as a fever, and then told you to return the next day to see if this first reading was right? Reading core temperature is no different than a surface recording taken under proper thermal imaging guidelines. Either the information taken on the first thermogram is valuable or the technology is unstable and useless. Research following patients for over 5 years has proven that the thermal patterns and differential temperatures at the surface of the body are remarkably stable and held within a very narrow range. These research studies were used to establish the normative database to which we compare patients when reading thermograms. Thermovascular patterns are as unique as a fingerprint and can be followed with accuracy for decades. It is when there is a change to this stable thermal fingerprint that a problem is signaled.
This begs the question as to why patients are being asked to return in 3 months. I would ask one of these offices for at least one peer-reviewed and published research paper demonstrating the need for this in order to establish a stable baseline. The research has already been done. In the early days of thermography each set of thermal images were taken in triplicate. The patient was acclimated in a temperature controlled imaging room under standard protocols for 15 minutes and then imaged. The patient would then be left for another 15 minutes and imaged again. This was finally repeated once more. In these early days thermologists were unsure about the stability of the process and the possibility of changes. Once the stability of the thermal data was established this practice was stopped. Then, as mentioned above, this was taken a step further by watching the thermal stability of patients for over 5 years. Studies have proven that a single set of thermal images taken under proper guidelines is completely accurate for analysis.
Under the established standards and guidelines for medical infrared imaging, recalling patients for follow-up thermograms is based solely on clinical need. When it comes to breast thermography, follow-up thermograms are performed based on the known metabolism of breast cancers. Under these guidelines each breast must be graded into one of 5 thermobiological (TH) categories. The level of TH grading acts as an individualized risk assessment based on the patients own biology. Depending on the TH grading, and taking into consideration the metabolism of breast cancers, the patient will be asked to return in a reasonable amount of time.
Since it was established over 30 years ago that a single thermogram is all that is needed for immediate analysis, you might want to ask yourself why are some offices having all their initial thermogram patients return in 3 months?
Who interprets the images?
A very special skill set is needed to interpret these thermal emission patterns. It takes years of study along with an understanding of embryology, neurophysiology, biochemistry, functional systems, and abnormal metabolic processes to produce a clinical thermologist. Within the healthcare specialties, Doctors of Chiropractic (DC), Medical Doctors (MD), and Doctor of Osteopathy (DO) can take additional training and obtain the necessary clinical acumen to specialize in Thermography.
Our group of independent thermologists can trace their lineage back to some of the original researchers, professors, and association founders. All of our doctors have undergone a quality education in clinical thermology that encompassed many hours of post-graduate classroom instruction, a supervised field residency, hundreds of sets of images co-read by a thermologist instructor, written examinations and a practical imaging examination before earning their board certification.
Do I still need a mammogram?
Patient Choice Ultrasound and Thermography does not radiation scare or mammogram shame it’s clients.
Women choose to have thermograms for many reasons. Your thermographer is unable to advise you whether you should have a mammogram. This is something you need to discuss with your health care provider and decide what is right for you yourself.
It has been determined that no one method of examination alone will serve all the needs in early breast cancer detection (1,2,6). Thermography’s role is in addition to mammography, not in lieu of. Thermography does not replace mammography and mammography does not replace thermography, the tests complement each other. Proper use of breast self exam, physician exams, thermography, and mammography together provide the earliest detection system available today (3,7,8). If treated in the earliest stages, cure rates greater than 95% are possible (3,6).
Until such a time as there is a cure for breast cancer, progress must be made in the fields of early detection coupled with sound clinical decision-making.
A doctor’s referral is not needed to have a thermogram.
Thermography Services:
Thermography is a non – invasive and painless approach to your personalized breast health risk assessment.
Thermography is based on the principle that metabolic activity and vascular circulation in both pre-cancerous tissue and the area surrounding a developing breast cancer is almost always higher than in normal breast tissue. In an ever-increasing need for nutrients, cancerous tumors increase circulation to their cells by holding open existing blood vessels, opening dormant vessels, and creating new ones (neoangiogenesis). This process frequently results in an increase in regional surface temperatures and vascular patterning of the breast. MIR uses ultra-sensitive medical infrared cameras and sophisticated computers to detect, analyze, and produce high-resolution images of these temperature variations and vascular patterns. Because of MIR’s sensitivity, these thermovascular variations may be among the earliest signs of breast cancer or a pre-cancerous state of the breast (3,6,7,8,9).
Studies also show that an abnormal infrared image is the single most important marker of high risk for developing breast cancer, 10 times more significant than a family history of the disease (5). Consequently, in patients with a persistent abnormal thermogram, the examination results become a marker of higher future cancer risk (4,5). Depending upon certain factors, re-examinations are performed at appropriate intervals to monitor the breasts. This gives a woman time to take a pro-active approach by working with her doctor to improve her breast health. By maintaining close monitoring of her breast health with the combined use of screening imaging, self-breast exams, clinical examinations, and thermography, a woman has a much better chance of detecting cancer at its earliest stage and preventing invasive tumor growth.
*Physicians order not needed
*Please follow protocol prior to appointment
The applications of Thermography are broad and range from simple soft tissue injury to a risk assessment marker for breast cancer. It is important to note that infrared imaging, like other imaging procedures (e.g. CT, MRI, mammography, ultrasound) does not provide a diagnosis. Infrared imaging cannot be used as a “body scan” to search for metastasis (the spread of cancer) or internal organ pathologies. There are many other tests that can provide true screening (early detection) for these conditions – Thermography cannot. Infrared imaging is not a stand-alone test, but an additional procedure that your doctor can use along with other tests to evaluate your health. The following list is just some of the conditions that have associated infrared thermal emission markers:
Altered gait manifestations
Arteriosclerosis (peripheral)
Brachial Plexus Injury
Breast Disease
Bursitis
Carotid Artery Stenosis
Carpal Tunnel Syndrome
Chronic pain
Compartment Syndromes
Complex Regional Pain Syndrome (CRPS)
Dental Irritation/Inflammation
Diabetes (secondary complications)
Disc Syndromes (spinal discogenic pain)
Facet Syndrome
Fibromyalgia
Headache Evaluation (e.g. cervicogenic, migraine, sinus)
Herniated Disc/Ruptured Disc
Hypesthesia
Hyperaesthesia
Inflammation
Intervertebral Disc Disease
Ligament Tears
Lumbosacral Plexus Injury
Muscular Spasm
Muscle Tears
Myofascial Irritation
Myofascial Pain Syndrome
Nerve Entrapment
Nerve Impingement/Pressure
Nerve Root Irritation
Nerve Stretch Injury
Neuritis
Neuropathy
Neurovascular Compression
Osteoarthritis
Paresthesia
Peripheral Nerve Abnormalities
Pinched Nerves
Referred Pain Syndromes
Reflex Sympathetic Dystrophy (RSD)
Repetitive Strain Injuries
Raynaud’s Disease
Rheumatoid Arthritis
Sacroiliac Ligament Tear
Sacroiliac Syndrome
Sensory Nerve Abnormalities
Sinus Irritation/Inflammation
Skin Conditions
Soft Tissue Injury
Spinal Cord Injury
Sports Injuries
Strain/Sprains
Superficial Vascular Disease
Synovitis
Temporal Arteritis
Tendonitis
Thoracic Outlet Syndrome
Thyroid Conditions
TMJ Dysfunction (TMD)
Trigeminal Neuralgia
Trigger Points
Whiplash Conditions
And many more …
*Physicians order not needed
*Please follow protocol prior to appointment
